Cataracts are one of the most common ailments of an aging population, manifesting in the fifth or sixth decade of life. This condition, which leads to blurred or cloudy vision, is caused by proteins that break down in the lens of our eyes, forming an increasingly opaque mass. Although cataracts can cause blindness if untreated, they can be treated with a simple surgery to remove the aging lens. In the U.S. alone, more than 4.5 million people undergo the procedure each year with great success.
For a small population of those patients, however, surgery replaces one problem with another. The oxidative stress from the surgical procedure damages sensitive endothelial cells that line the back surface of the cornea. Even under normal conditions, these cells are slow to heal. But in people with pre-existing corneal disease or advanced cataracts, the insult to the cornea from surgery is larger than usual, leading to corneal edema that can defocus light coming into the eye. This creates visual impairment that may lead to long-term follow-up treatment and compromised daily activities. If severe enough, the only remaining treatment option would be a full corneal transplant, a procedure that may restore vision, but requires patients to take immunosuppressant drugs for the rest of their lives.
Supporting corneal healing with TTHX1114: An enhanced form of FGF1
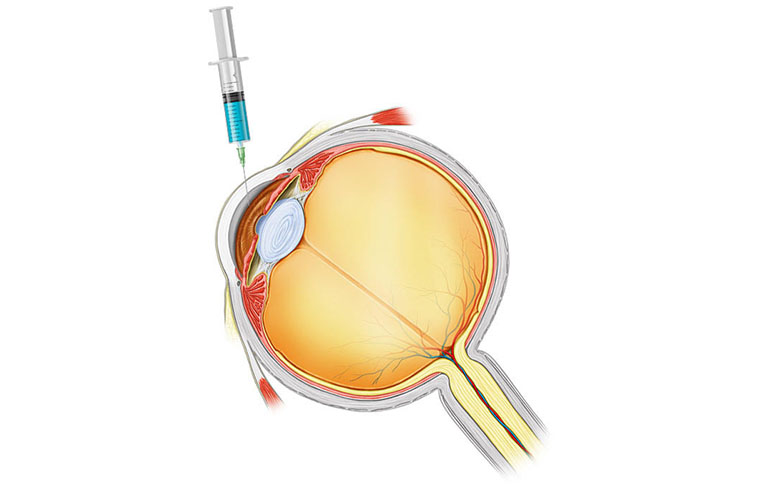
Trefoil Therapeutics is working to improve outcomes in patients who experience corneal edema. A new investigational therapy developed by Trefoil, called TTHX1114, has been shown to stimulate natural cellular processes that protect the corneal cells from damage and improve the rate at which those tissues heal. Clinical trials with high-risk patients demonstrated that a single injection of the drug into the eye lowered recovery times from several months to an average of 4.2 weeks, with no serious adverse events.
The promising results observed in clinical trials may be due in large part to the drug’s origins. TTHX1114 is a modified version of a naturally-occurring growth factor called FGF1 (Fibroblast Growth Factor 1), a protein that serves as one of the main catalysts for cell division in the cornea. FGF1’s normal role is to protect cells from damage such as oxidative stress and to facilitate healing of tissue. Unfortunately, native FGF1 is quite unstable and has a very short duration of biological activity.
 Overcoming FGF1 instability with TTHX1114
Overcoming FGF1 instability with TTHX1114
Increasing the amount of FGF1 present in the eye would theoretically improve healing—and indeed, several other groups of researchers have explored therapeutic versions of the protein for use in dermal wounds. These efforts, however, have been stymied by issues with the molecule’s stability. Since FGF1 breaks down easily, using it to promote growth in the cornea might require near-daily injections into the eye, a procedure few patients would be willing to tolerate.
For this reason, Trefoil engineered TTHX1114 to alter the properties of the native protein, making it less fragile, more persistent in the eye, and better able to bind to cell receptors in the cornea. After mapping the three-dimensional structure of FGF1, we were able to analyze and model a number of weak points in its molecule. Several regions of the protein contain an amino acid called cysteine, which can be easily oxidized, causing the carefully-folded structure of the protein to unravel and break apart.
Engineering resilience
In TTHX1114, these amino acids have been replaced with similar structures that are less prone to oxidation. Trefoil has also improved the way that the molecule folds, reducing the amount of free space available within its structure. By pushing its amino acids closer together, the protein becomes tighter and more robust.
In addition to these improvements, Trefoil also inserted a new internal bond between two distant parts of the protein chain, locking the structure of TTHX1114 into place so that it cannot unfold. These changes greatly increase the overall stability of the drug, allowing it to remain in the eye long enough for effective receptor binding to create a therapeutic effect.
Preserving natural function and enhancing delivery
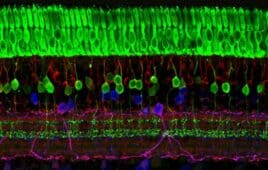
The improvements to the FGF1 molecule used to create TTHX1114 were carefully created to retain all the natural functions of FGF1 including binding to tissue, protection of cells from oxidative stress and other insults, and acceleration of healing of tissues. Trefoil has demonstrated the potent protective and proliferative effects of TTHX1114 on corneal endothelial and epithelial tissues in preclinical models and in human clinical trials.
At the moment, Trefoil is developing two different delivery systems for TTHX1114. The first, an intracameral injection directly into the eye which targets endothelial cells on the back of the cornea; the second, a topical eye drop solution, can reach epithelial cells on the cornea’s outer surface. Unlike corneal cells inside the eye, these epithelial cells naturally regenerate on a regular basis, however, there are a number of conditions in which the healing process can be long and painful, and may lead to corneal scarring which causes lifelong degradation in vision. Topical TTHX1114 could reduce this pain and minimize the risk of long-term harm by accelerating recovery from the corneal damage associated with a number of conditions.
This two-program pipeline can address conditions affecting the front and back of the cornea—a part of the body that currently has few new treatment options. By advancing these two innovative programs, Trefoil can offer ophthalmologists new pharmacologic treatments to provide a better standard of care, and improve the vision of millions of people who have limited treatment options today.
David Eveleth is president and CEO of Trefoil Therapeutics, a clinical-stage biotech company that seeks to restore vision in millions of people with corneal disease.
Filed Under: Ophthalmology