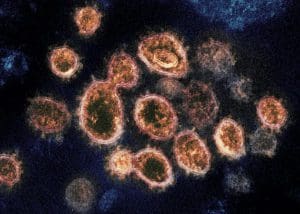
This transmission electron microscope image shows SARS-CoV-2 – the virus that causes COVID-19 – isolated from a patient in the U.S. Image courtesy of NIAID
Last year, herd immunity seemed like a comforting promise as researchers worked on dozens of COVID-19 vaccine candidates and a silver-lining to the rampant spread of the virus — the more people who got infected, the more natural immunity that would develop over time.
There are now dissenting opinions about how the term relates to the current pandemic and the role of vaccines in achieving it.
A Wall Street Journal op-ed recently opined that herd immunity is just around the corner, thanks mainly to natural immunity. Meanwhile, former FDA commissioner Dr. Scott Gottlieb and The Atlantic argued the U.S. might never reach herd immunity against SARS-CoV-2. Meanwhile, the consulting firm McKinsey suggests that herd immunity could be within reach in late 2021.
“Herd immunity in a little under a month is unrealistic, and probably not the message people need to be hearing right now,” Johns Hopkins Assistant Professor of Emergency Medicine Lauren Sauer recently told Bloomberg.
The Brazilian city of Manaus could also point to the difficulty of sustaining herd immunity from infection alone. A majority of the population there had been infected as of October, but the emergence of the antibody-resistant P.1 variant fueled a surge of cases there in January.
The British Journal of Medicine recently mused that Manaus might be the final nail in the coffin for natural herd immunity.
But data elsewhere suggest that natural immunity and measures such as social distancing are effective. COVID-19 cases are falling in the U.S. and many other countries.
“COVID-19 cases have been declining for five weeks,” said CDC director Rochelle Walensky at a recent media event. In the past week, the seven-day average of cases decreased nearly 29%.
Even countries that were hard-hit by more-transmissible variants such as the U.K., South Africa, Denmark and Switzerland have seen substantial declines in COVID-19 cases.
Infections in Brazil, driven in large part by an exceptionally infectious variant, remain stubbornly high.
Swift declines in COVID-19 cases elsewhere and accelerating vaccine administration provide hope that at least temporary herd immunity is possible. Imperial College London researcher Alexandra Hogan concluded that a vaccine that was 90% effective would need to be administered in at least 55% of a population to induce temporary herd immunity, assuming social distancing and widespread mask-wearing continue.
In the U.S., more than 75 million vaccine doses have been delivered, and approximately 64 million doses have been administered. “This represents more than 44 million people who have received at least one dose of the COVID-19 vaccine and approximately 20 million people who are fully vaccinated, receiving two doses,” Walensky said.
Ultimately though, given the vague definitions of “herd immunity” and “even pandemic,” it may be more helpful in the interim to focus on controlling the spread of the virus so that it doesn’t hamper routine activities. A growing number of experts are beginning to stress that eradicating the virus will be nearly impossible. There is, however, hope for bringing “the virus sufficiently under control,” as vaccine pioneer Dr. Paul Offit recently told The Atlantic.
Filed Under: Uncategorized



