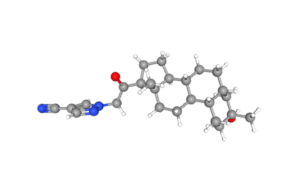
Zuranolone molecule image from PubChem
Sage Therapeutics has pegged the wholesale acquisition price of the oral postpartum depression (PPD) drug Zurzuvae (zuranolone) at $15,900 for a 14-day course of the therapy. The drug, co-developed by Biogen, won the FDA green light in August. The companies plan on launching the drug in December. The DEA has classified zuranolone as Schedule IV, which mostly includes benzodiazepines. That status could influence prescriber and patient perceptions concerning the drug’s safety profile and potential for abuse. The formulary review process for Zurzuvae, critical for insurance coverage, will occur throughout 2024.
Sage had initially aimed to price Zurzuvae under $10,000, but its failure to win approval earlier this year for zuranolone for major depressive disorder altered its pricing strategy.
Zurzuvae postpartum depression cost in context
The wholesale acquisition cost (WAC) of Sage Therapeutics’ Zurzuvae is significantly higher than that of SSRIs, commonly prescribed off-label for PPD treatment. While healthcare providers pay the WAC, patient costs vary based on insurance coverage. For example, the out-of-pocket cost for generic fluoxetine (20 mg per day) is approximately $16 a month for uninsured patients, whereas the brand-name Prozac can cost around $534 per month without insurance. In contrast, Sage’s Zulresso, an IV treatment for PPD, has a WAC of $34,000, not including the additional costs of hospitalization required to administer the medication
To justify the cost, Sage points to a 2017 model that concluded that the multi-year average cost of untreated perinatal mood and anxiety disorders per mother-child pair was $31,800. It points to estimates that one in eight mothers with live births experience PPD.
The company noted that Zurzuvae is the only oral option specifically for PPD, and that the drug has the potential for rapid and sustained improvement in depressive symptoms based on the SKYLARK and ROBIN studies. In those trials, investigators noted benefits as early as the third day and maintained through the forty-fifth. Sage also noted that the drug, which has a novel mechanism of action as a neuroactive steroid and GABAA receptor positive modulator, can be administered on its own or adjunctively with oral antidepressants. It also noted that the drug was generally well-tolerated in trials.
The phase 3 SKYLARK and ROBIN trials provide quantitative evidence supporting the efficacy of Zurzuvae. In the SKYLARK study, for instance, 57% of women treated with the neuroactive steroid achieved at least a 50% reduction in depressive symptoms by day 15. This percentage increased to 61.9% by day 45. In comparison, only 38% and 54.1% of women in the placebo group had similar improvements at those time points. The ROBIN study further supported these findings, with 72% of participants on zuranolone demonstrating improvement in PPD symptoms after 14 days, a significant margin over the 48% in the placebo group.
Market analysts weigh in on Zurzuvae’s pricing
Some analysts expected a higher price point for Zurzuvae, including Piper Sandler and Truist. Truist Securities, while maintaining a “hold” rating for Sage, remains cautious owing to the underwhelming performance of Sage’s previously launched PPD drug, Zulresso. The firm also adjusted their financial model for Sage, reflecting a conservative forecast for Zulresso sales as a result of potential cannibalization from Zurzuvae.
Assessing Zurzuvae’s value in PPD treatment
Ultimately, whether Zurzuvae is worth it for a given patient hinges on the severity of PPD symptoms, the efficacy of alternative therapies, including the off-label use of SSRIs, and the patient’s financial and insurance situation. In terms of the efficacy of SSRIs for PPD, data are mixed. One systematic review found that SSRIs appear to be more effective than placebo in treating PPD in terms of response and remission rates, but the quality of evidence is low. A meta-analysis of three randomized controlled trials (RCTs) comparing SSRIs to placebo found that women who received SSRIs were more likely to show symptom improvements (52.2% versus 36.5%) or achieve remission (46.0% versus 25.7%) at follow-up. A systematic review of placebo-controlled randomized data from six randomized controlled studies indicated that antidepressants may be superior to placebo in treating postpartum depression, but, the authors noted low certainty of evidence.
For context, phase 3 trials of zuranolone in PPD found that 72% of participants on zuranolone found improvement in PPD symptoms after 14 days, a significant margin over the 48% in the placebo group. By contrast, SSRI’s mode of action is more gradual, typically requiring a period of 6 to 8 weeks to assess their effectiveness.
Given the high economic burden of PPD and the condition’s impact on the baby and family, zuranolone could offer significant quality-of-life improvements for PPD patients. The formulary review process scheduled for 2024 will be critical in determining Zurzuvae’s accessibility to a broader patient population. In the meantime, the decision to prescribe Zurzuvae will largely hinge on individual considerations, including clinical outcomes, potential side effects, and the patient’s specific situation
Filed Under: clinical trials, Drug Discovery, Neurological Disease, Obstetrics & gynecology



