Lion Biotechnologies, Inc.’s LN-144 achieved a 29 percent objective response rate in a study of patients with advanced metastatic melanoma.
The biotechnology company presented the new data from an ongoing Phase II melanoma study evaluating its lead immunotherapy candidate LN-144 at the 2017 ASCO Annual Meeting in Chicago.
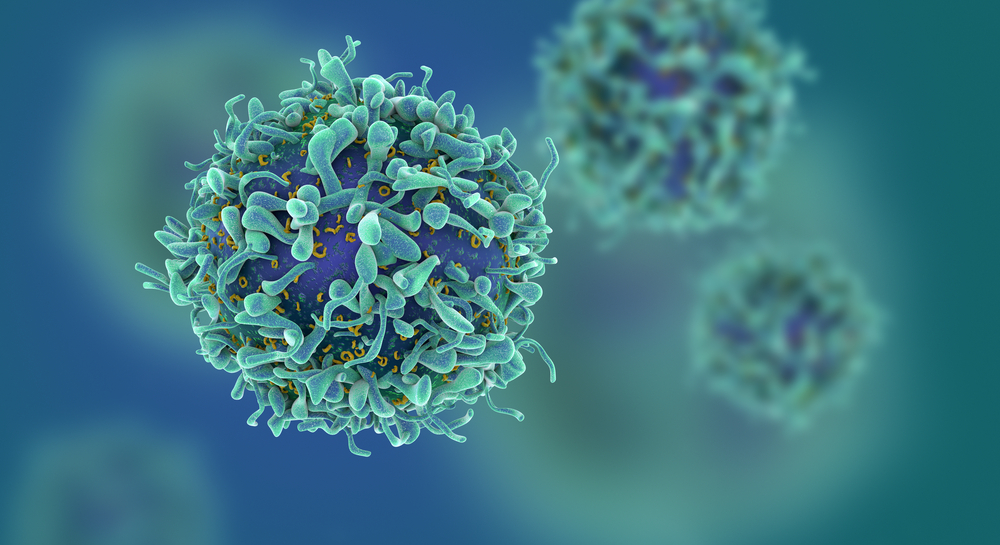
LN-144, Lion’s tumor-infiltrating lymphocytes (TIL), is an autologous, ready-to-infuse cell therapy that has demonstrated distinctive efficacy in the treatment of metastatic melanoma.
TILs is potentially applicable to all solid tumors, including ovarian, colorectal, head and neck, and other cancers.
The Phase II, multicenter, three-cohort study is designed to assess the safety and efficacy of LN-144 for treatment of patients with metastatic melanoma. Cohorts one and two will enroll up to 30 patients each and cohort three is a re-treatment cohort for a second LN-144 infusion in up to ten patients.
The first two cohorts are evaluating two different manufacturing processes for LN-144, according to the company. Patients in cohort one are receiving fresh, non-cryopreserved TIL and cohort two patients are receiving product manufactured through a more streamlined and rapid three-week procedure yielding a cryopreserved product.
Study findings
Results showed cell therapy with TILs is an effective treatment with an acceptable safety profile for advanced metastatic melanoma patients who are refractory to anti-PD1 therapies.
Sixteen patients from cohort one with advanced metastatic melanoma who have failed at least one prior systemic therapy were enrolled to receive LN-144, followed by IL-2.
Patients had a median age of 55 and all had prior anti-PD1 and a majority (88 percent) had anti-CTLA4 therapy.
“Eighty-one percent of the patient population had stage IV disease with a median number of three therapies and a median number of four lesions present at enrollment, which is fairly high,” said Maria Fardis, CEO of Lion Therapeutics in an email to Drug Discovery & Development. In addition, she said about half of the patients had elevated LDH levels, which is a poor prognosis factor for outcome of cancer patients in general.
Among the 16 patients, an objective response rate of 29 percent was reported including one complete response continuing beyond 15 months post-administration of a single TIL treatment. Seventy-seven percent had a reduction in target tumor size.
Responses were observed in patients with tumors carrying wild type or BRAF mutations.
In Phase II clinical trials conducted at National Cancer Institute (NCI), patients treated with this product demonstrated an objective response rate of 56%.
“Patients in earlier line of therapy as well as late line have been investigated and found to respond. The response in earlier lines with TILs have been higher at over 50 percent, per NCI, and somewhat lower in later line of therapy—as Lion is enrolling–at around 30 percent, said Fardis. “We continue offering this trial to patients who have failed prior anti-PD1 which is an approved therapy and BRAF inhibitors if BRAF mutant.”
The most common non-hematologic grade 3-4 treatment emergent adverse event was hypophosphatemia and no neurotoxicity of grade 3 or higher was reported. There were no deaths or discontinuations due to serious adverse events related to study treatment
In addition, the researchers found TIL products can be centrally manufactured for broad clinical application. Based on that finding, the ongoing trial will be expanded to enroll more patients and will have a shorter manufacturing process as well as offering retreatment for study patients.
Filed Under: Drug Discovery




