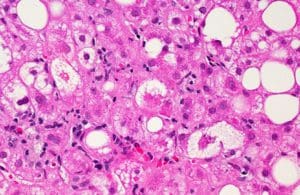
Liver with signs of nonalcoholic fatty liver disease. Image courtesy of NIH.
Although nonalcoholic steatohepatitis (NASH) is one of the most common types of chronic liver disease in the U.S., it is a disease that is unfamiliar to many Americans. Despite this, its prevalence is increasing, and by some estimates, 27 million Americans will be living with NASH by 2030.
NASH is a progressive condition that starts with excess fat buildup in the liver, leading to inflammation and liver damage. While the cause of NASH is unknown, it is associated with a broader set of metabolic disorders. Important risk factors include elevated triglyceride or cholesterol levels, type 2 diabetes, high blood pressure and obesity, particularly with body fat concentrated around the waist. NASH is also more prevalent in certain ethnic groups, including Asian and Hispanic populations. While there are generally no symptoms until late in the disease process, the initial inflammation often leads to fibrosis (scarring) of the liver, which can progress to cirrhosis (advanced, late-stage scarring). Patients who develop cirrhosis are at risk for complications, including liver failure and liver cancer (hepatocellular carcinoma).
Since no FDA-approved drug for the treatment of NASH is available, physicians currently focus on treating the underlying risk factors noted above, including type 2 diabetes or obesity. Many drugs, however, are being investigated for potential utility in NASH and advances are urgently needed to address this rapidly growing global health problem.
Using mitochondria-based therapeutics to treat NASH
In 2007, CohBar, Inc. created the category of mitochondria-based therapeutics, building on the work of the company’s founders, Dr. Pinchas Cohen and Dr. Nir Barzilai. In 2001, Cohen Barzilai discovered a class of peptides encoded within the mitochondria that affect metabolic regulation and protection. One of the key early insights that led to the development of CohBar’s novel platform of mitochondria-based therapeutics was the recognition that the effects of some of these mitochondrially-encoded peptides were not limited to local regulation within the mitochondria but could have important roles to play in critical biological pathways quite distinct from what is traditionally acknowledged as mitochondrial function. CohBar is using this novel approach to develop analogs of these natural peptides to treat various serious systemic conditions, focusing on diseases involving inflammation and fibrosis, including NASH and idiopathic pulmonary fibrosis (IPF). As analogs of naturally occurring peptides, we expect our product candidates to have better safety and tolerability profiles than other drug development approaches.

CohBar researchers at the Menlo Park lab working on the research and development of mitochondria-based therapeutics.
Recently, CohBar completed a successful multi-center, randomized, double-blind, placebo-controlled clinical study of CB4211, a first-in-class mitochondria-based therapeutic, for the potential treatment of NASH and obesity. In addition to showing that CB4211 appeared safe and well-tolerated, the data indicated robust and significant improvements in markers of liver damage. In this four-week study of 20 obese subjects with fatty liver disease, we demonstrated statistically significant reductions compared to placebo in both ALT (alanine aminotransferase) and AST (aspartate aminotransferase), enzymes that are normally present in liver cells and released into the blood when the liver is damaged. The reductions seen after treatment with CB4211 indicate decreased liver injury — the ultimate goal when treating NASH patients. Further, the level of improvement in ALT was comparable or superior to that seen with other competing products under development for NASH.
Additional data from the study demonstrated a statistically significant decrease in glucose levels compared to placebo and a trend towards lower body weight with CB4211 treatment. Finally, we saw a meaningful reduction in the level of liver fat, though this was roughly comparable to the decrease seen in the placebo group. The reductions in glucose levels are particularly encouraging since only one of the subjects in this study had diabetes. Considering almost 50% of NASH patients have diabetes as a comorbidity, the potential to lower glucose levels raises intriguing possibilities for combination therapy in diabetic NASH patients. Combination therapy involving CB4211, CohBar’s product candidate, is particularly attractive since its mechanism of action is unique amongst the NASH field. In addition, our preclinical work demonstrated synergies between CB4211 and common diabetic treatments such as the GLP-1 agonist semaglutide (sold under the brand Ozempic).
Based on the data generated to date, we believe we have a unique therapy that has the potential to provide substantial benefits for this underserved growing epidemic. Beyond the implications for CohBar’s CB4211 program, the clinical trial results validate our overall approach to therapeutic peptide development. CohBar now has evidence that analogs of peptides encoded within the mitochondrial genome can have significant beneficial impacts on relevant disease processes in human subjects. The results also confirm the company’s hypothesis that analogs of these naturally occurring peptides are likely to have superior safety and tolerability profiles.
CohBar’s scientists have spent years mining the mitochondrial genome, discovering more than 100 natural peptides, and generating over 1,000 novel analogs, representing a substantial opportunity for future product development. In the near term, the company plans to work with disease experts to determine the best path forward for CB4211 while continuing to advance CB5138-3, the company’s second clinical candidate, into the clinic. CB5138-3 is a different peptide than CB4211, and it has impressive anti-fibrotic and anti-inflammatory properties. CohBar is initially developing this product candidate to treat IPF, another serious condition with significant morbidity and mortality.

Dr. Joseph J. Sarret
It is clear that an FDA-approved treatment for NASH is desperately needed. NASH is currently the second leading cause of liver transplantation in the United States. The persistent increase in the rates of obesity and type 2 diabetes will further exacerbate the burden of liver disease in the coming years. Given the absence of any FDA-approved therapeutics to treat NASH, the American Liver Foundation advises a variety of tactical recommendations, including weight loss, eating a healthy diet with limits on sugar and salt and regular exercise, as well as drinking coffee to reduce the risk of liver fibrosis and taking Vitamin E, an antioxidant, which may mitigate or neutralize inflammation damage. While these tactics have not been proven to cure NASH, they may moderate its impacts as we await the arrival of the first FDA-approved medication.
About the Author
Dr. Joseph J. Sarret is chief executive officer and director of CohBar Inc., (NSDQ:CWBR), a clinical-stage biotechnology company focused on the research and development of mitochondria based therapeutics, an emerging class of drugs for the treatment of chronic and age-related diseases. He can be reached at: joe.sarret@cohbar.com.
Filed Under: Drug Discovery





Tell Us What You Think!
You must be logged in to post a comment.