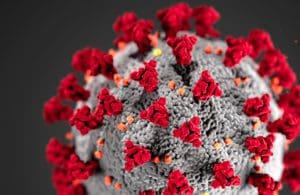
[Image courtesy of CDC]
Dexamethasone is a corticosteroid commonly used for treating arthritis and other cases of inflammation. In total, 2,104 patients were randomized in Oxford’s trial to receive dexamethasone in doses of 6 mg, once per day, either by mouth or intravenous injection, over the course of 10 days.
The patients receiving the steroid were compared with 4,321 patients randomized to receive usual care alone. Among the usual care patients, 28-day mortality was highest in those who required ventilation (41%), intermediate in patients only requiring oxygen (25%) and lowest among those who did not require respiratory intervention (13%).
According to a news release, dexamethasone reduced deaths by one-third in ventilated patients and by one-fifth in other patients receiving oxygen, while no benefit was observed among patients who did not require respiratory support.
Researchers said that, based on the results, one death would be prevented by the treatment of around eight ventilated patients or around 25 patients requiring oxygen alone. They are working to publish the full details of the study “as soon as possible.”
United Kingdom chief scientific adviser Sir Patrick Vallance said in the release that the news is exciting as dexamethasone is inexpensive and widely available.
“Dexamethasone is the first drug to be shown to improve survival in COVID-19,” Oxford professor of emerging infectious diseases and one of the trial’s chief investigators Peter Horby said. “This is an extremely welcome result. The survival benefit is clear and large in those patients who are sick enough to require oxygen treatment, so dexamethasone should now become standard of care in these patients. Dexamethasone is inexpensive, on the shelf, and can be used immediately to save lives worldwide.”
According to a BBC report, the researchers concluded that, had dexamethasone been used to treat U.K. patients from the start of the pandemic, up to 5,000 lives could have been saved. That same report said the U.K. government stockpiled 200,00 courses of the drug and the National Health Service will make it available as a treatment for patients on ventilators and oxygen.
Meanwhile, in the U.S., the FDA is now warning that two drugs that have been used in the treatment of COVID-19 may not interact safely and could reduce effectiveness of treatment.
Investigational antiviral drug remdesivir, which received emergency use authorization for treating COVID-19 patients, may have its antiviral activity reduced when co-administrated with hydroxychloroquine. The FDA said in a statement that it is not aware of instances of this reduced activity occurring in the clinical setting, but is evaluating data related to remdesivir.
“Over the course of this unprecedented pandemic, the FDA has issued emergency use authorizations for a variety of medical products after evaluating the available scientific evidence and carefully balancing any known or potential risks against the benefits of making these products available during the current public health emergency,” FDA Center for Drug Evaluation & Research acting director Dr. Patrizia Cavazzoni said in the release. “We understand that, as we learn more about these products, changes may be necessary based on new data – such as today’s updates for health care providers about a potential drug interaction and other important information about using remdesivir to treat COVID-19 patients.
“As we have done throughout the pandemic, the FDA continues to evaluate all of the emergency use authorizations issued and their related materials and will continue to make changes as appropriate based on emerging science and data.”
Just yesterday, the FDA announced that it revoked its EUA that allowed doctors to use the malaria drugs hydroxychloroquine and chloroquine to treat COVID-19, citing concerns about the drugs’ efficacy against the virus. The agency said that a large, randomized clinical trial in hospitalized patients found the malaria medicines showed no benefit for decreasing the likelihood of death or speeding recovery.
Filed Under: clinical trials, Drug Discovery, Drug Discovery and Development, Infectious Disease





Tell Us What You Think!
You must be logged in to post a comment.