Through one of the largest studies yet of Alzheimer’s disease (AD) patients and their brothers, sisters, and children, researchers at Mayo Clinic Jacksonville have found strong evidence that genes other than the well-known susceptibility risk factor APOE4 influence who is at risk for developing the neurodegenerative disease later in life.
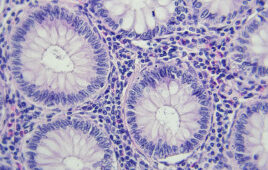
Studying 25 multigenerational families of individuals diagnosed with late onset Alzheimer’s disease (LOAD), the most common form of the disorder, as well as hundreds of other participants, the research team found that blood levels of amyloid beta (Aß) proteins associated with AD were significantly elevated compared to protein found in non-blood relatives, such as spouses.
These first-degree relatives were cognitively normal and age 65 or less—many of them too young for symptoms of LOAD to show up.
“These results indicate that genetic factors of substantial magnitude lead to significant elevations of Aß in the blood of asymptomatic, young individuals from extended LOAD families,” says the study’s lead investigator, Nilufer Ertekin-Taner, M.D., Ph.D. “This fits with our hypothesis that Ab levels rise years before development of the disorder.”
The researchers have already identified three candidate genes on chromosome 10 that is associated with LOAD, and at least one of them, the gene that produces insulin degrading enzyme (IDE), is now regarded as a prime candidate for contributing to the disease. IDE degrades both insulin and amyloid protein, and scientists hypothesize that when there is too much insulin in the brain such as due to diabetes or lower expression levels of IDE, this may lead to toxic accumulation of Aß.
The results, which first appeared online in October of last year, will be published in the Feb. 19 issue of Neurology.
Release date: January 17, 2008
Source: Mayo Clinic
Filed Under: Genomics/Proteomics