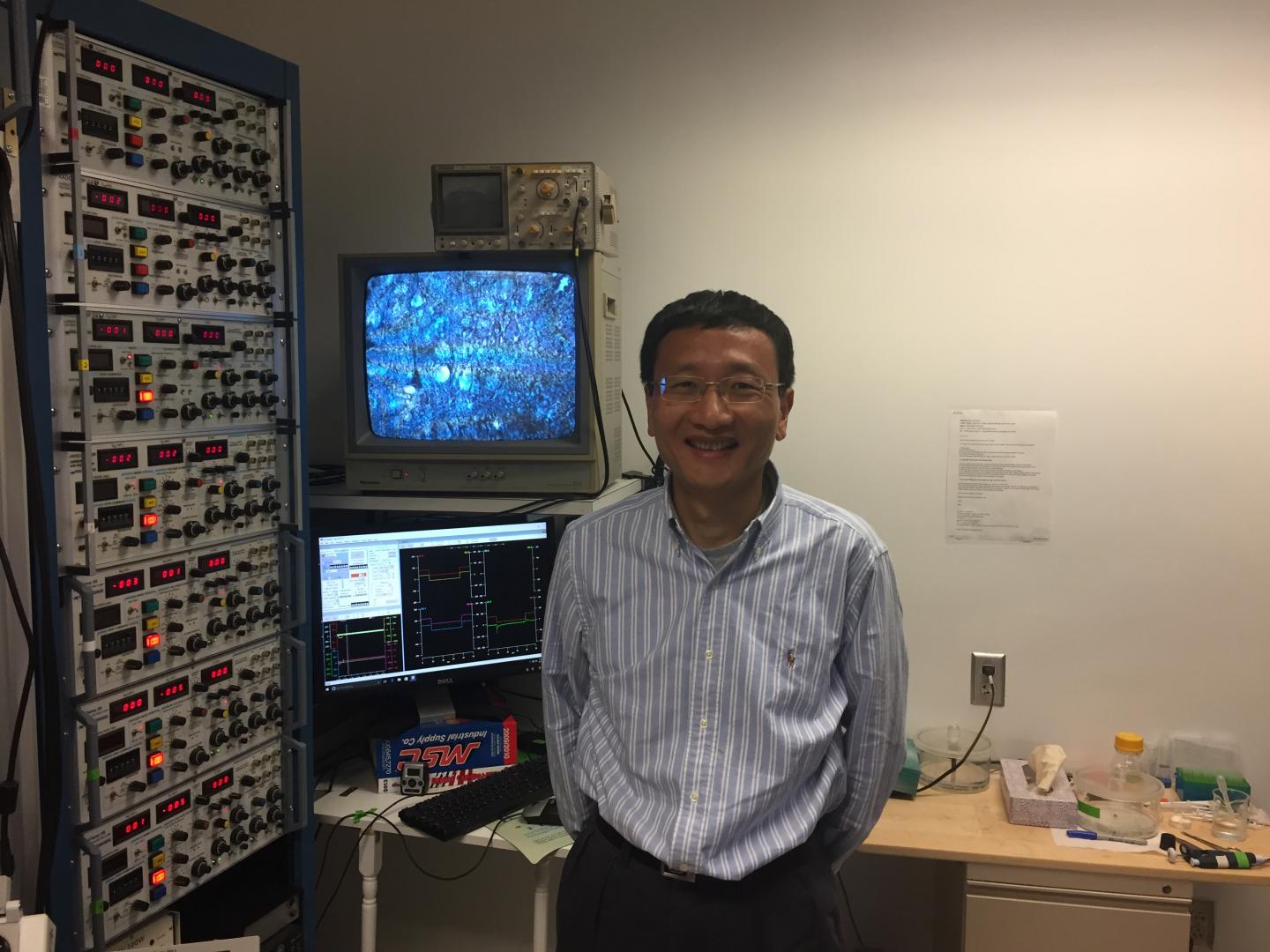
J. Julius Zhu, Ph.D., of the University of Virginia School of Medicine, led the team that developed a new technique that can let a single cancer research lab do the work of dozens. Source: Josh Barney | UVA Health System
A new technique developed at the University of Virginia School of Medicine will let a single cancer research lab do the work of dozens, dramatically accelerating the search for new treatments and cures. And the technique will benefit not just cancer research but research into every disease driven by gene mutations, from cystic fibrosis to Alzheimer’s disease – ultimately enabling customized treatments for patients in a way never before possible.
The new technique lets scientists analyze the effects of gene mutations at an unprecedented scale and speed, and at a fraction of the cost of traditional methods. For patients, this means that rather than thinking about the right drug for a certain disease, doctors will think about the right drug to treat the patient’s specific gene mutation.
“Every patient shouldn’t receive the same treatment. No way. Not even if they have the same syndrome, the same disease,” said UVA researcher J. Julius Zhu, PhD, who led the team that created the new technique. “It’s very individual in the patient, and they have to be treated in different ways.”
Understanding Gene Mutations
Understanding the effect of gene mutations has, traditionally, been much like trying to figure out what an unseen elephant looks like just by touching it. Touch enough places and you might get a rough idea, but the process will be long and slow and frustrating. “The way we have had to do this is so slow,” said Zhu, of UVA’s Department of Pharmacology and the UVA Cancer Center. “You can do one gene and one mutation at a time. Now, hopefully, we can do like 40 or 100 of them simultaneously.”
Zhu’s approach uses an HIV-like virus to replace genes with mutant genes, so that scientists can understand the effects caused by the mutation. He developed the approach, requiring years of effort, out of a desire to both speed up research and also make it possible for more labs to participate. “Even with the CRISPR [gene editing] technology we have now, it still costs a huge amount of money and time and most labs cannot do it, so we wanted to develop something simple every lab can do,” he said. “No other approach is so efficient and fast right now. You’d need to spend 10 years to do what we are doing in three months, so it’s an entirely different scale.”
To demonstrate the effectiveness of his new technique, Zhu already has analyzed approximately 50 mutations of the BRaf gene, mutations that have been linked to tumors and to a neurodevelopmental disorder known as cardio-facio-cutaneous syndrome. The work sheds important light on the role of the mutations in disease.
Rescuing Failed Treatments
Zhu’s new technique may even let researchers revisit failed experimental treatments, determine why they failed and identify patients in which they will be effective. It may be that a treatment didn’t work because the patient didn’t have the right mutation, or because the treatment didn’t affect the gene in the right way. It’s not as simple as turning a gene on or off, Zhu noted; instead, a treatment must prompt the right amount of gene activity, and that may require prodding a gene to do more or pulling on the reins so that it does less.
“The problem in the cancer field is that they have many high-profile papers of clinical trials [that] all failed in some way,” he said. “We wondered why in these patients sometimes it doesn’t work, that with the same drug some patients are getting better and some are getting worse. The reason is that you don’t know which drugs are going to help with their particular mutation. So that would be true precision medicine: You have the same condition, the same syndrome, but a different mutation, so you have to use different drugs.”
Filed Under: Drug Discovery




