 Interest in ketamine and psilocybin as potential therapies for mood disorders has surged since around 2010. A groundbreaking 2000 study at Yale revealed the powerful antidepressant effects of ketamine, a dissociative anesthetic. Unlike traditional antidepressants which can take weeks or months to have an impact, a single dose of ketamine led to significant improvements in depressive symptoms in as little as 72 hours.
Interest in ketamine and psilocybin as potential therapies for mood disorders has surged since around 2010. A groundbreaking 2000 study at Yale revealed the powerful antidepressant effects of ketamine, a dissociative anesthetic. Unlike traditional antidepressants which can take weeks or months to have an impact, a single dose of ketamine led to significant improvements in depressive symptoms in as little as 72 hours.
Structural neuroplasticity and non-hallucinogenic psychoplastogens

Kurt Rasmussen
This revelation, which Kurt Rasmussen, chief scientific officer of Delix, described as a “watershed development” in neuropsychiatry, helped spark a new understanding of the brain’s capacity for rapid structural neuroplasticity. Drugs like ketamine can promote the formation of new connections between neurons, a process known as synaptogenesis. “Neuron damage is a component of many different disease states,” Rasmussen noted. “And the discovery of ketamine’s rapid structural neuroplasticity is a watershed development in neuropsychiatry.”
Following the discovery of ketamine’s ability to prompt rapid structural neuroplasticity, research on classical psychedelics such as LSD, DMT, psilocybin and mescaline has found similar effects on brain plasticity. “We’re discovering that the commonality between these compounds is this rapid change in structural neuroplasticity,” Rasmussen said, “which is remarkable as it shows that the brain has the capacity and capability to do that quickly.”
Rasmussen said the field of neuropsychiatry is “entering a whole new realm” of exploring the use of therapies that can promote rapid and enduring effects for mood disorders. “In addition, COVID has not only increased the rates of depression and anxiety but also significantly escalated the rates of substance use disorders,” he said.
Elevated rates of mood disorders contribute to the surging research interest in ketamine, classic psychedelics and related compounds for mood disorders. The line graph below reflects the rapid acceleration in the number of studies exploring the use of ketamine for potential to alleviate the symptoms of various mood disorders.

Interest in ketamine and esketamine is ramping up given its potential in mood disorders. [Data from PubMed]
Non-hallucinogenic psychoplastogens: Safe alternatives for neuroplasticity
But ketamine and classic psychedelics also present risks. Ketamine has a history of misuse and when administered in high chronic doses, can result in cognitive deficits, hepatotoxicity, damage to the bladder and other problems. Similarly, clinical trials specifically focused on classic psychedelics tend to contraindicate the substances for individuals who have a family history of psychosis or schizophrenia. In the 1960s, the misuse of the classic psychedelic LSD played a significant role in heightening concerns about the safety and potential misuse of these substances, contributing to their restrictions in the following years. In light of these potential hazards, the research and development of non-hallucinogenic psychoplastogens offer a promising alternative.
In 2022, a collaborative research team from UNC-Chapel Hill, UC San Francisco, Yale, Duke and Stanford developed a new compound that targets the 5-HT2A serotonin receptor, the same receptor targeted by psychedelic drugs. This breakthrough, in line with the development of non-hallucinogenic psychoplastogens, has the potential to trigger antidepressant effects without the associated hallucinogenic experience.
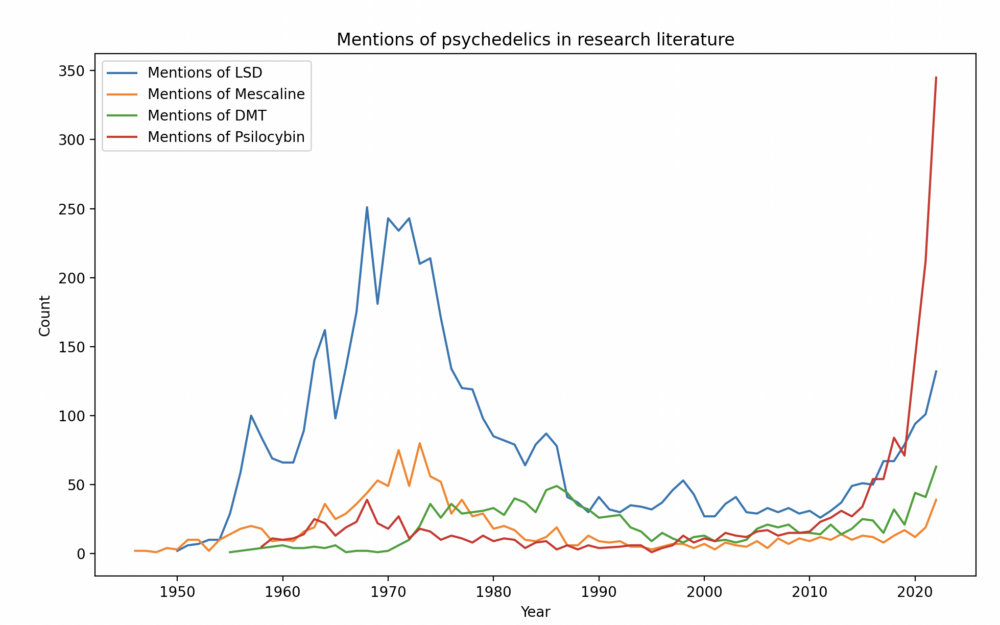
Research on classic psychedelics, especially psilocybin, has accelerated recently. [Data in image above from PubMed]
Delix Therapeutics focused on non-hallucinogenic psychoplastogens
This research aligns with the mission of Delix Therapeutics, a company focused on non-hallucinogenic psychoplastogens. These drugs foster the growth of neural connections, and in May 2023, Delix initiated a phase 1 study of DLX-001. This drug is one of many non-hallucinogenic psychoplastogens that the company is exploring. “We’re designing these psychoplastogens to make the structural neuroplastic change without producing some of the other effects, such as hallucinations or the other effects of ketamine,” Rasmussen added.
The future of neuropsychiatry with non-hallucinogenic psychoplastogens
Rasmussen envisions a future where compounds like DLX-001, a non-hallucinogenic psychoplastogen that promotes neuroplasticity without inducing hallucinations, could benefit a wider patient population, including those with schizophrenia and dementia. “What it represents to me is finally addressing pathophysiology in neuropsychiatry,” he said.
One promising feature of DLX-001 is its potential for intermittent use, as opposed to daily medication. “It seems like, perhaps DLX-001 could be used more intermittently, as needed, which would be a significant change in how those conditions are treated,” Rasmussen said. This approach is not entirely new, as some patients already take ketamine intermittently as part of an off-label treatment for mood disorders. Biogen and Esai are seeking FDA approval for zuranolone, an intermittent neuroactive steroid therapy that could potentially be used to treat major depressive disorder (MDD) and postpartum depression.
Rasmussen believes we are on the brink of a new era in neuropsychiatry, in which non-hallucinogenic psychoplastogens like DLX-001 could help neuropsychiatry move beyond symptom management. “I genuinely feel like we’re starting to treat the disease now, not just symptoms,” he said. The hope is that compounds like DLX-001 will not require daily administration and will have enduring effects on patients’ mental health.
Filed Under: Brain Breakthroughs, clinical trials, Drug Discovery, Drug Discovery and Development, Neurological Disease, Psychiatric/psychotropic drugs, Regulatory affairs




Tell Us What You Think!
You must be logged in to post a comment.