It has been just over two decades since the first nanoparticle-based therapy was FDA approved for the treatment of cancer.
In that time, the field has grown and matured significantly, attracting the interest of an increasing number of researchers across multiple disciplines, said Piotr Grodzinski, PhD, the Chief of Nanodelivery Systems and Devices Branch at the Cancer Imaging Program of the National Cancer Institute (NCI).
“I have this plot that shows the number of publications per year within nanotechnology in medicine and it was close to zero in year 2000,” said Grodzinski in an interview with R&D Magazine. “Today there are about 20,000 papers written on this topic each year. A lot of researchers are starting to work in this area and we (the NCI) are receiving large number of grant applications concerning the use of nanomaterials and nano-devices in novel cancer interventions. In last three years there has been two FDA approvals of new nanoparticle-based treatments and a multitude of clinical trials.”
Initial demonstrations
The first nanoparticle-based treatment to be FDA approved for cancer was Doxil—a formulation of the chemotherapy agent doxorubicin delivered via the nanoparticle material liposome. The agent, approved in 1995, has the benefit of a reduced side effect profile compared to its traditional counterpart—delivery of free doxorubicin. While patients treated longer term with doxorubicin often develop cardiomyopathy— the weakening of the heart muscle—patients treated with Doxil do not typically develop the same side effect.
Another nanoparticle-based, Abraxane, was FDA approved in 2005. Abraxane is a nanoparticle albumin–bound formulation of another chemotherapy, paclitaxel, which is used to treat several types of cancer including breast, lung, and pancreatic. The albumin-formulation eliminated the need for an organic solvent— required for delivery of free paclitaxel—thus eliminating solvent-related side effects.
“Historically, initial demonstrations were basically taking an established chemo-therapeutic, which was already approved by the FDA, and combining it with a nanoparticle,” said Grodzinski. “When you deliver it using a nanoparticle vehicle, you essentially modify the pharmacokinetics of the drug molecule because it is now attached to the particle. That increases its residence in blood circulation and can potentially contribute to an increase in the accumulation of nanoparticle-drug construct in the tumor.”
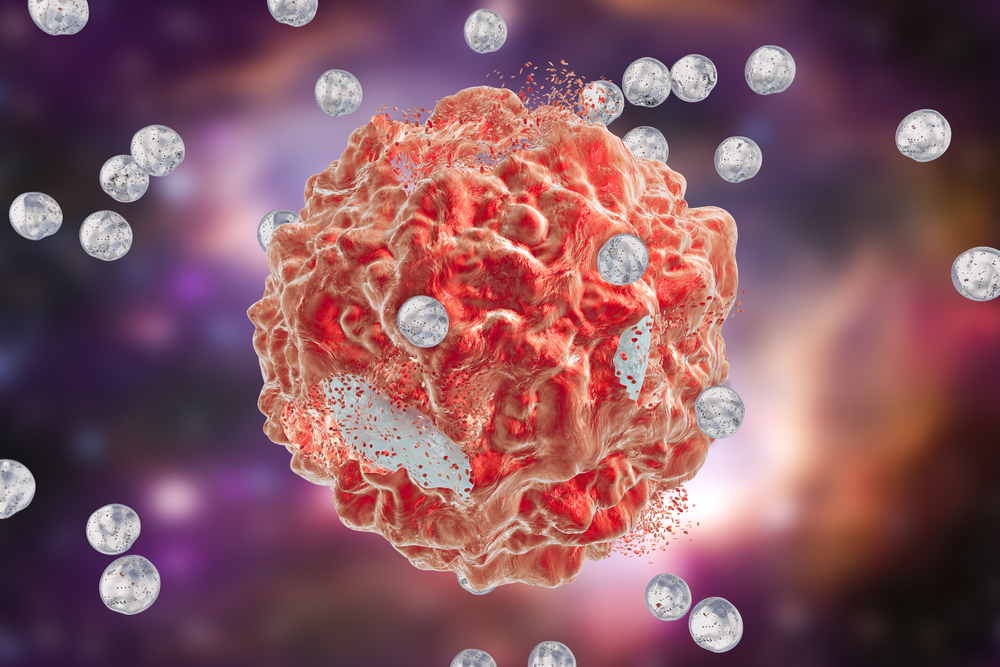
Nanoparticles are extravasated from blood flow into the tumor due to the so-called Enhanced Permeability and Retention (EPR) effect. This process is also called ‘passive tumor targeting’ since specific tumor targeting ligands are not used. The website of the NCI Alliance for Nanotechnology in Cancer program describes the EPR effect below.
“As tumor mass grows rapidly, a network of blood vessels needs to expand quickly to accommodate tumor cells’ need for oxygen and nutrient. This abnormal and poorly regulated vessel generation (i.e. angiogenesis) results in vessel walls with large pores (40 nm to 1 um); these leaky vessels allow relatively large nanoparticles to extravasate into tumor masses. As fast growing tumor mass lacks a functioning lymphatic system, clearance of these nanoparticles is limited and further enhances the accumulation. Through the EPR effect, nanoparticles larger than 8 nm (between 8-100 nm) can passively target tumors by freely pass through large pores and achieve higher intratumoral accumulation.”
This approach is considered “passive,” as nanoparticles do not use ligands targeting specific epitopes on the cell surfaces.
Active targeting
While passive targeting has proven to be effective, in more recent years, researchers have also begun investigating more complex designs known as “active targeting,” with the goal of creating more effective, next-generation nanoparticle therapeutics. This approach could enable certain modalities of therapies not achievable with EPR.
The NCI’s website describes active targeting as “the targeting of nanoparticles to tumor cells, microenvironment or vasculature, as well as directed delivery to intracellular compartments, through nanoparticle surface modification with small molecules, antibodies, affibodies, peptides or aptamers.”
At this time it is unclear if active targeting will be a game-changer in nano-drug delivery, said Grodzinski.
“I don’t think there is a definite answer on if active targeting will dramatically changes tumor accumulation of nanoparticles or not, since adding additional elements on particle surfaces modifies their characteristics,” he said.
Combination approaches
After initial successes using nanoformulations to reduce treatment side effects, researchers have started investigating more sophisticated nano-approaches, with the goal of creating treatments that are more effective than corresponding conventional therapies.
Combination nanoformulations are showing significant promise, said Grodzinski.
Several combination treatments have recently gained FDA approval. In 2013, Abraxane (nanoparticle albumin–bound formulation of paclitaxel) was approved in combination with gemcitabine for metastatic pancreatic cancer. In 2015, Onivyde—a similar combination therapy involving irinotecan liposome injection in combination with fluorouracil and leucovorin—was approved for the second-line treatment of patients with metastatic pancreatic cancer.
Another combination nano-formulation treatment, Vyxeos, was approved in Aug. 2017. Vyxeos is made up of daunorubicin and cytarabine— both chemotherapy agents—formulated with the nanomaterial liposome; it was approved for the treatment of acute myeloid leukemia (AML).
All three agents showed a modest increase of efficacy as compared to existing treatments, said Grodzinski.
“We need to look more broadly at combination therapies; they are strong area of interest now” said Grodzinski. “The recent demonstrations show the promise of combining more than one drug into delivery in a single nanoparticle. But, this can be taken further by combining different modalities of treatment, chemotherapy and radiation, for example, where one or both modalities would rely on nanoparticles.”
Up-and-coming areas of interest
Immunotherapy—leveraging a patient’s own immune system to fight cancer—is another area of oncology that has seen significant advancement in recent years. Numerous FDA-approved immunotherapies—such as Keytruda and Opdivo—have shown spectacular results, although the subset of the patient population responding to the treatment is still small. Nanotechnology is being investigated as a potential way to boost the effectiveness of immunotherapy.
“Everyone is interested in immunotherapy due to its recent success,” said Grodzinski. “The question now is, can the nanoparticles be effective delivery vehicles for vaccines or be used for for co-delivery of antigens and adjuvants? That is also an area of pretty strong interest.”
Researchers are investigating nanoparticles for delivery of immunostimulatory or immunomodulatory molecules in combination with chemo- or radiotherapy or as adjuvants to other immunotherapies. Stand-alone nanoparticle vaccines are also being designed to raise sufficient T cell response to eradicate tumors, through co-delivery of antigen and adjuvant, the inclusion of multiple antigens to stimulate multiple dendritic cell targets, and continuous release of antigens for prolonged immune stimulation. Molecular blockers of immune-suppressive factors produced can also be co-encapsulated in nanoparticle vaccines to alter the immune context of tumors and improve response.
Researchers are also looking at the potential of nanotechnology to develop new formulations that are not based on established and approved drugs. Nanotechnology could be used to reformulate drug molecules which were too toxic to be delivered in a free form, said Grodzinski.
“Researchers are considering the reformulation of APIs (active pharmaceutical ingredients) which are too toxic to deliver safely alone, but could benefit from nanoparticle formulation and gain wider therapeutic window to be delivered more safely,” he said.
Material scientists are also working to continuously improve and develop new nanomaterials beyond widely used liposomes or polymer-based particles. Newly developed particles could possess higher drug loading capacity, could provide altered biodistribution profiles, or be targeted.
Collaboration is key
Despite dynamic progress and the rapidly growing community of researchers involved in cancer nanotechnology research, there is still a lot to be accomplished in the field, said Grodzinski.
“The main focus now is to search for techniques allowing for increased accumulation of nanomedicines in the tumor which should potentially allow for higher efficacy and in parallel thinking about more sophisticated constructs which are capable of interacting with the tumor microenvironment,” he said. “I think everybody is still searching for that blockbuster nano-drug that will make everybody gasp.”
Close interactions of scientists from fields across biology, medicine and physical sciences are key to continued and further success of the field, said Grodzinski.
Many universities have set up interdisciplinary institutes, where researchers of different disciplines work side-by-side.
“These efforts lead to convergence of different disciplines and training of researchers who can move more freely between different disciplines than before,” said Grodzinski.
NCI funded several large centers of Cancer Nanotechnology Excellence at academic institutions across the country. Cross-disciplinary collaboration has had a positive impact there as well, said Grodzinski
“We’ve looked at the publication profiles of researchers working there; those who were publishing primarily in technology and materials development in the past migrated to biomedical applications through collaborating with their colleagues working in biology and clinical labs. The opposite also happened, biologists gained interest in how to leverage novel materials for biological purposes,” he said. “Such long term, collaborative interactions are paying off, leading to the gelling of the nanomedicine community.”
Filed Under: Drug Discovery




