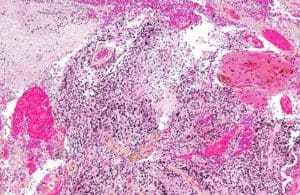
Intermediate magnification micrograph of a glioblastoma. HPS stain image courtesy of Wikimedia.
The emerging biopharmaceutical company Global Cancer Technology (GCT; San Diego) is developing a novel x-ray–activated modality for drug delivery to treat glioblastoma, which remains stubbornly difficult to treat.
GCT has a licensing agreement with the University of California, San Diego (UCSD) for a drug delivery platform that unites a nanocrystal to a prodrug that can be activated using radiosurgery. GCT has also acquired two patents for investigational drugs that can cross the blood-brain barrier. One is an inhibitor of phosphatidylinositol 3-kinase (PI3K), a type of enzyme involved in several cellular functions that facilitates rapid growth in glioblastoma. The other compound targets Vps34, a phosphatidylinositol 3-kinase. Both compounds modulate autophagy, a regenerative cellular process. According to UCSD researchers, autophagy yields amino acids that support tumor survival.
 Early research involving a collaboration between GCT and the Barrow Neurological Institute (Phoenix) indicates that inhibiting phosphatidylinositol 3-kinase enzymes may also alert the immune system to the presence of glioblastoma. “The results so far are preliminary but promising in that arena,” said M. Karen Newell-Rogers, a chief scientific consultant and advisor for the company.
Early research involving a collaboration between GCT and the Barrow Neurological Institute (Phoenix) indicates that inhibiting phosphatidylinositol 3-kinase enzymes may also alert the immune system to the presence of glioblastoma. “The results so far are preliminary but promising in that arena,” said M. Karen Newell-Rogers, a chief scientific consultant and advisor for the company.
But while PI3K inhibitors have shown promise in glioblastoma cultures, researchers have had less success using them in vivo given the challenge of homing in on the glioblastoma site. For that reason, GCT is using a nanotechnology-based drug delivery approach to target the tumor site.

Bob Proulx
“The goal is to concentrate that therapeutic effect, potentially use less of the drug and have a more efficacious effect because you’ve localized it to the site of the tumor,” said Bob Proulx, president and CEO of Imagion Biosystems. He is also an advisor to GCT.
To that end, GCT has licensed novel scintillator technology from UCSD. For context, a scintillator is a chemical entity that emits light when exposed to certain radiation spectra. GCT is experimenting with using a linker to conjoin a drug and nanoparticle. The linker is cleavable when a photon strikes it. “Once I know the particles are at the diseased tissue, I can hit them with a low dose of gamma radiation,” Proulx said. Then, using a radiosurgery tool such as a Gamma Knife, a surgeon can trigger the release of the drug. “That’s what makes this combination so unique,” Proulx added. It could combine a molecule that potentially targets a key growth mechanism in glioma and a mechanism for releasing it at the site where it is needed.
The approach is broadly similar to the use of antibody-drug conjugates (ADCs), small molecule drugs attached to an antibody intended to bind to and thus target cancer cells. One drawback to ADCs, however, is that “it’s often difficult to get antibody conjugates past the blood-brain barrier,” as Newell-Rogers explained.
Another potential problem with ADCs, though, relates to the bio-functionality of the antibody. If an ADC binds to a receptor on a cell, “your therapeutic payload may have been delivered, but it may be sitting there on the surface of the cell membrane,” Proulx said. This is because the ADC must be absorbed to have a therapeutic effect. “What’s novel about the GCT nano-scintillator particle is that it acts as a carrier,” Proulx added.
Once the drug reaches the tumor area, an external mechanism such as a Gamma Knife can activate it. “You can localize the gamma knife just to the place where you want the drug released,” Newell-Rogers said. “So you don’t have a lot of the toxicity issues that you have when you’re using a drug that could have activity all over the body.”
Filed Under: Drug Delivery, Drug Discovery





Tell Us What You Think!
You must be logged in to post a comment.