A group of genomics researchers are looking in an unlikely place in an effort to better predict individual risk of deadly diseases.
Scientists from the Primary Care Research Network and Center for Bioinformatics and Genetics at the Edward Via College of Osteopathic Medicine (VCOM), are investigating , so-called junk DNA—genomic DNA that does not encode proteins, but whose function is not yet fully understood by scientists—to gain more insight into the human genome. Harold “Skip” Garner, PhD, the executive director of VCOM, explained in an exclusive interview with R&D Magazine, that junk DNA is often neglected in the field, but in reality, it can shed light on a person’s overall health.
“All the other groups out there spend their time looking for what are called single nucleotide polymorphisms (SNPs),” he said. “The truth is they really haven’t worked out very well. There’s a big gap between the amount of genetic variations and the amount of genetic associations we know exists. For most cancers, nothing is known because everyone is focused on the SNPs.”
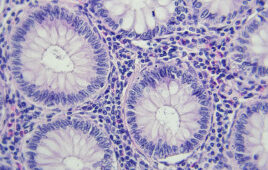
Non-coding DNA or junk DNA, is DNA that results from the movement of sections of DNA to different positions within the genome. Most of these regions contain several copies of transposons—sequences that copy or cut themselves out of one part of the genome and reinsert themselves in another part.
Garner said that most researchers disregard junk DNA as being not vital to understanding genomics.
Genomic medicine involves looking at a patient’s genome—their complete set of DNA, including all genes—as part of their clinical care. This emerging medical discipline could be particularly useful in oncology, pharmacology, rare and undiagnosed diseases and infectious disease.
Because there is so much data available in the human genome, doctors often have difficulty ciphering through and coming up with a clear and concise conclusion.
The researchers previously found that the human genome contains undiscovered genes and DNA sequences that play a role in both cancer and aging.
Garner said the starting point of their research is extensive genomic databases, such as The Cancer Genome Atlas, the 1000 Genome Project and the Harvard Personal Genome Project that are readily available to study.
“We download thousands and thousands of genomes and these are healthy genomes and cancer genomes, autism, Alzheimer’s, it doesn’t matter,” he said. “Lots of people have focused on analyzing genomes before, so there are tens of thousands available. So we download them and we do something that no one else does, we look at the junk DNA.”
Through this new focus, the team is working to develop a test that will enable doctors to take either a mouth swab or a blood sample from a patient and decipher the risk of the 200 different known cancers, as well as other diseases and disorders like autism and Alzheimer’s disease.
Garner said they have validated the test for lung cancer, as well as for a number of cancers. The new approach has been licensed to Orbit Genomics, a company co-founded by Garner.
In a 2017 study, the researchers used their genomic test to successfully predicted the genotype for 105 out of 119 microsatellite markers that significantly differ in the lung cancer germline samples compared to the non-cancer controls.
Garner explained that they are using a similar approach with complex multigenic diseases such as heart disease and neurological disease. They have already demonstrated its use in heart disease with a test for that determines if patients are likely to respond to a particular drug that is used to treat Atrial fibrillation.
The researchers have already found new genetic markers for autism and Alzheimer’s and are now working to refine and verify them.
The researchers have already demonstrated that they can integrate many disease risk diagnostics into a single test.
“We are basically looking at all of the genetics of all of the very complex diseases,” Garner said. “Cancer, heart disease and neurological disease are hard to study because they are complex, thousands of genes participate.”
According to Garner, there is a major knowledge gap when it comes to cancer, largely because most researchers have been focused on the SNPs. In fact, he said that despite being the most studied cancer with the most known about it, there still is only about 40 percent known about breast cancer.
Garner explained how other researchers end up getting it wrong.
“All the current algorithms get it wrong, so when they try to reconstruct the sequence, they get it wrong,” he said. “They get it right 20 percent of the time and you can’t make discoveries with 80 percent noise. We have figured out how to get to about 95 percent accurate and have been analyzing every sequence we can get.”
With so much data at hand, the researchers are hoping the aid of supercomputers will allow them to pinpoint a specific genomic mutation that led to a patient’s cancer.
“Two people that have the same cancer may look the same, but it may be caused by two completely different sets of mutations,” Ramu Anandakrishnan, PhD, an assistant professor of biomedical sciences at VCOM, said during the interview. “That’s one of the reasons why a cure that may be effective for one person isn’t effective for another person. So the idea is if we can identify which of the four or five mutations causes the cancer in person A then we can focus our treatment on those mutations.”
Along with the risk factor test, the researchers hope to develop a diagnostic companion that will tell whether a patient will respond to a certain drug and whether that drug will harm the patient. This type of test will eliminate some adverse effects for patients taking certain drugs, while reducing the trial and error process of deciding what the best drug to take is for that given patient.
Genomics and precision medicine may become increasingly important as the emerging popularity of companies like 23andMe, which offers customers a complete genetic history that ultimately could be used to access a person’s risk factor for various diseases.
For example, African American women tend to have a larger risk of a more deadly form of breast cancer than Caucasian women do.
“In precision medicine really you are employing their individual genome against what they are doing and your genome tells you about your ethnicity background and overall summary of the risk of getting these diseases,” Garner said. “For the most part we still don’t understand what the genome does but we tell doctors to be prepared when your patient walks in. You have to be able to condense it down into very specific reports.
“VCOM is preparing our new doctors for the new world of precision medicine and we are developing [continuing medical education] courses for existing doctors.”
Filed Under: Genomics/Proteomics