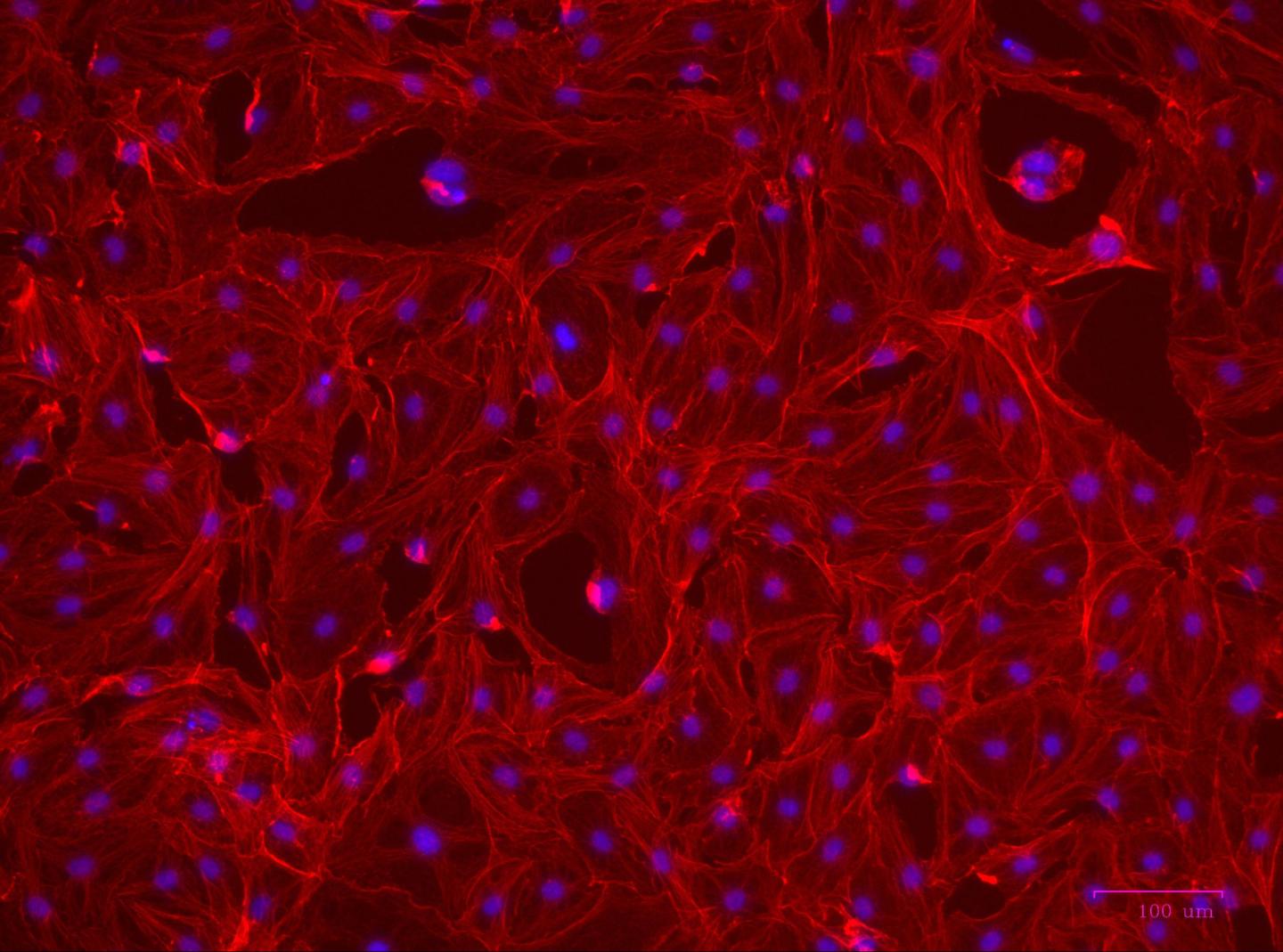
In thyroid eye disease (TED), orbital fibroblasts form contractile myofibroblasts that secrete high levels of collagen and lead to destructive tissue remodeling. Fluorescent staining shows the myofibroblast morphology of orbital fibroblasts from a TED patient. Cells were stained with the actin binding molecule, phalloidin (red) and nucleic acid stain, DAPI (blue). Source: The American Journal of Pathology
A new class of therapies may be on the horizon for thyroid eye disease (TED) and other destructive scarring conditions. At least 50% of patients with Graves’ disease, an autoimmune disease that primarily attacks the thyroid gland, develop eye problems including inflammation, discomfort, scarring, and bulging eyes. Abnormal over-production and activation of collagen-producing myofibroblasts underlie many of these conditions. A new study published in The American Journal of Pathology found that activation of the aryl hydrocarbon receptor (AHR) pathway by its ligands blocks collagen production and myofibroblast proliferation in TED.
“Currently there are no effective therapies for TED that target or prevent the excessive scarring and tissue remodeling. Our studies reveal that AHR is a novel target for treatment of this disease and potentially other diseases that manifest with excessive scarring,” explained lead investigator Richard P. Phipps, PhD, of the Department of Environmental Medicine and Flaum Eye Institute of the School of Medicine and Dentistry of the University of Rochester (Rochester, New York).
The primary goals of the research were to better understand the molecular pathways underlying scarring in TED and to control or prevent tissue remodeling or destruction. The orbital remodeling in TED is likely induced by infiltrating T lymphocytes and mast cells, which activate orbital fibroblast effector cells to either proliferate and form scar-producing cells called myofibroblasts or turn into pro-inflammatory fat cells. Myofibroblasts produce large amounts of extracellular matrix material such as collagen, are contractile, and secrete a variety of cytokines and chemokines, all of which enhance scar formation.
The investigators focused on studying the activity of AHR, a transcription factor that is known to play a key role in regulating inflammatory and immune responses, and the effects of two AHR ligands (ITE and FICZ). Previous research had shown that AHR activation decreases transforming growth factor beta (TGFβ), a cytokine that induces myofibroblast formation. When human orbital fibroblasts from TED patient tissue were compared to tissue from patients without TED, the researchers discovered that TED orbital fibroblasts expressed higher levels of AHRs than non-TED orbital fibroblasts.
The AHR ligands turned on AHR-dependent genes and blocked the TGFβ-driven transformation of human orbital fibroblasts to scar-forming myofibroblasts. The ligands also interfered with other aspects of TED tissue remodeling including collagen production, filament formation, and myofibroblast contraction. Importantly, the ligands impaired myofibroblast function without affecting cell viability.
“We also showed for the first time that AHR signaling in primary human orbital fibroblasts disrupts the pro-fibrotic Wnt/β-catenin pathway, which is important for scar cell formation,” noted Dr. Phipps. Wnt/β-catenin has been shown to play a crucial role in other fibrotic diseases such as pulmonary fibrosis and hypertrophic scar formation.
“We are excited that our translational research team of clinicians and basic researchers have come together to present these novel findings and hope that future studies and trials based on this work can move forward to bring targeted therapies for TED,” commented Dr. Phipps.
Each year, approximately one million Americans are diagnosed with Graves’ eye disease. Symptoms may range from irritation and dryness to characteristic protrusion of the eyes, eyelid retraction, vision impairment, light sensitivity, and blindness in the most severe cases. Symptoms can be managed by artificial tears for dryness, prednisone for double vision, radiation therapy to reduce swelling and double vision, or surgical decompression. Smoking is known to exacerbate TED.
Filed Under: Drug Discovery




