Celgene and Agios Pharmaceuticals started the month on a positive note.
Their new therapy for a subset of patients with AML has been approved by the U.S. Food and Drug Administration (FDA) ahead of its PDUFA date at the end of August.
The FDA granted approval for enasidenib (Idhifa) for adult patients with relapsed or refractory AML (R/R AML) with an isocitrate dehydrogenase-2 (IDH2) mutation as detected by an FDA-approved test.
Enasidenib is the first and only FDA-approved therapy for patients with R/R AML and an IDH2 mutation—which represents between 8 and 19 percent of AML patients—and it’s the first drug approval for Agios Pharmaceuticals, who partnered with Celgene to develop the targeted therapy.
The treatment is approved for use with a companion diagnostic, the Abbott RealTime IDH2 Assay, which is used to detect specific mutations in the IDH2 gene in patients with AML.
If the IDH2 mutation is detected in blood or bone marrow samples using the assay, the patient may be eligible for treatment with enasidenib. The drug, which is an isocitrate dehydrogenase-2 inhibitor, works by blocking several enzymes that promote cell growth.
“The FDA approval of Idhifa provides the first-ever treatment option for patients living with relapsed or refractory AML and an IDH2 mutation. We appreciate the FDA’s efforts to expedite the availability of Idhifa for patients with this devastating disease weeks ahead of the PDUFA date,” said Mark Alles, Chief Executive Officer of Celgene. “This milestone further illustrates the value of Celgene’s unique distributed research model. Our partnership with Agios is an exceptional example of how Celgene and its collaborators can positively impact the lives of patients with high unmet needs.”
David Schenkein, M.D., Chief Executive Officer of Agios, adds: “The FDA approval of Idhifa just four years after entering the clinic is the first of what we expect to be multiple first-in-class precision medicines for patients with cancer and rare genetic diseases from our productive discovery engine. We look forward to working closely with Celgene to co-commercialize Idhifa and provide access for patients in the U.S. with this devastating disease.”
Approval pipeline
The accelerated approval was based on results from the phase I/II AG-221 AML-001 study including safety, rate and duration of complete response (CR) or CR with partial hematologic recovery (CRh) and rate of conversion to transfusion independence.
The single-arm trial of 199 patients with relapsed or refractory AML who had IDH2 mutations, as detected by the RealTime IDH2 Assay, measured the percentage of patients with no evidence of disease and full recovery of blood counts after treatment (complete remission or CR), as well as patients with no evidence of disease and partial recovery of blood counts after treatment (complete remission with partial hematologic recovery or CRh).
Enasidenib was given orally at a starting dose of 100 mg daily until disease progression or unacceptable toxicity. Reductions were provided to help manage side effects.
Nineteen percent of patients experienced CR for a median 8.2 months, and 4 percent of patients experienced CRh for a median 9.6 months. Among the 157 patients who required transfusions of blood or platelets due to AML at the start of the study, 34 percent no longer required transfusions after treatment with enasidenib.
Adverse reactions
Common side effects of the drug include nausea, vomiting, diarrhea, increased levels of bilirubin (substance found in bile) and decreased appetite. Women who are pregnant or breastfeeding should not take Idhifa because it may cause harm to a developing fetus or a newborn baby.
It also comes with a boxed warning that an adverse reaction known as differentiation syndrome can occur and can be fatal if not treated.
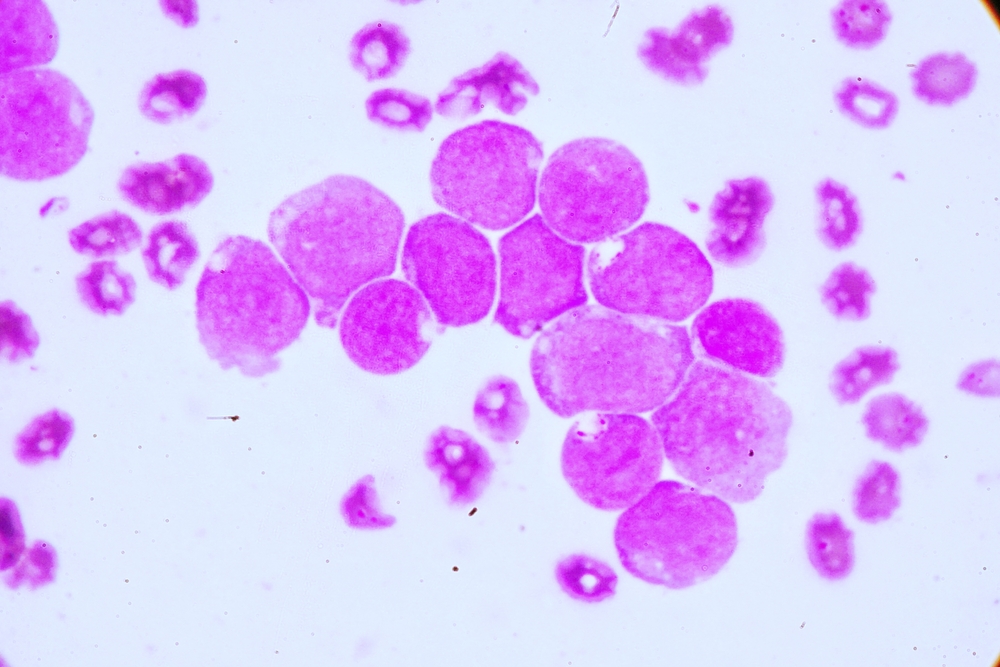
AML is a cancer of the blood and bone marrow marked by rapid disease progression and is the most common acute leukemia affecting adults with more than 21,000 new cases estimated in the U.S. each year.4,5,6 The majority of patients with AML eventually experience relapse. Relapsed or refractory AML has a poor prognosis. For 8 to 19 percent of AML patients, the mutated IDH2 enzyme blocks normal blood cell development and results in an overabundance of immature blood cells.
The drug was granted both a priority Review designation and Orphan Drug designation.
Filed Under: Drug Discovery




