Automated cell thawing and delivery maximizes the chances of therapeutic success. Image credit: MedCision
Cell and gene therapies offer the potential to treat and even reverse serious diseases such as heart failure, diabetes, and cancer, for which there is currently no known cure. After years of rigorous clinical testing, these unique “living medicines” are finally poised to make the leap from the realm of clinical research to the world of mainstream medicine. Cancer immunotherapies, and in particular, CAR-T cell therapy, are among the most clinically advanced of the cellular therapy treatments expected to earn FDA approval and advance to the commercial stage. To give these therapies their best chance of success, the cell and gene therapy industry needs to ensure that each step of the drug development and delivery process is as robust and cost-effective as possible.
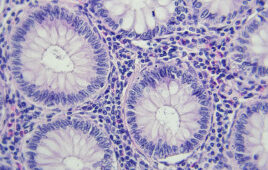
In manufacturing, the best way to standardize and streamline product development is to automate it, and cellular therapeutics are no exception. Living cells, however, pose manufacturing and delivery challenges that other drug products do not. Cells are uniquely responsive to their environment; highly sensitive to changes in factors such as temperature, storage media, and handling conditions. Therefore, each step of the cell therapy development process should be closely examined for optimization opportunities in order to maximize the chances for effectiveness in patients.
For practical and logistical reasons, cell therapies destined for commercial distribution are usually cryopreserved. Cryopreservation protects therapeutic efficacy by preventing metabolic processes that can age, alter or otherwise damage sensitive cells. Freezing cells ensures flexibility for patients and doctors, the ability to manufacture a treatment away from the hospital or clinic, distribution to multiple sites, and preservation of multiple doses of cells for future treatments. While the cryopreservation process has already been optimized, and to some extent automated, cryopreserved cells must also be thawed, a process which for the most part is neither optimized nor automated.
Cell thawing is still chiefly a manual process, using inconsistent methodologies dependent on the use of heated water baths, heat blocks, and bead baths. When a water bath is being used, the sample may be removed every thirty seconds or so to check on thaw progress. This interrupts heat influx and prolongs the thawing procedure, which can damage cells. Thawing times can be inconsistent depending on how busy the technician happens to be, or to what depth a cryobag or vial is submerged in the water. The variability inherent in non-automated cell thawing techniques can result in significant loss of viability or functionality downstream, detrimentally affecting patient outcomes.
Thawing is often the last step a cellular therapeutic undergoes before being administered to a patient, and its importance shouldn’t be overlooked. A carefully controlled thawing profile should allow for rapid thawing which traverses the transition to melting temperature as rapidly as possible, without proceeding so quickly that water influx from the surrounding freezing media bursts the cell. Ideally, cell type, membrane permeability, and freezing media composition should also be taken into account, since these factors all affect the optimal thawing profile. Automating the cell thawing process improves reproducibility and minimizes human error. It can also be used to avoid the contamination risk inherent to water bath use, and to incorporate an electronic interface for sample tracking and data collection. Certain models of automated dry thawers, notably the ThawSTAR CB system, incorporate single use technology, such as disposable contaminant isolation barriers, to eliminate the risk of cross contamination between therapeutics. These many benefits are encouraging the cell therapy industry to willingly adopt standardized thawing methods to give their clinical trials the maximum chance of success.
Cell thawing is just one example. Other elements of the cell therapy manufacturing and processing pipeline also offer challenges, and will benefit from further automation, and more robust, integrated methodologies. Cell culture and expansion is a prime example of this. Automated, bioreactor-based culturing systems are already standard at many cell manufacturing facilities, due to their cost-effectiveness and efficiency at streamlining production. Such bioreactor systems are often enhanced by the integration of single use disposable liners that significantly reduce the need for preparation and decontamination efforts. These systems can be either highly integrated or modular, lending themselves to the incorporation of new functions, like T-cell modification and activation.
The question of whether manufacturing should be centralized or decentralized is another major point of dialogue within the industry. Both approaches have their pros and cons. It’s certainly easier to assure product consistency in a centralized facility, which is a big plus when your product is a living cell capable of responding to changes in the environment. Even so, variability is inevitably introduced, either during cold chain handling, or at point of care, where products may be thawed and administered by differing methodologies.
Decentralized manufacturing facilities, on the other hand, are closer to (or at) point of care, and require shorter distribution chains. Such sites may be more suitable to single-patient directed, autologous therapies, especially where variability may be less of a concern, and time more so. Yet this decentralized approach has its own drawbacks. Establishing multiple manufacturing sites over a wide area is expensive. Without automation, it would be very difficult to maintain product comparability between sites, a factor which is vitally important for allogeneic therapies. Each cell therapy product has highly defined characteristics such as cell surface expression, antigen specificity, or immunosuppressive capability. These characteristics are expected to be virtually identical every time a patient is treated.
Depending on the treatment being produced, we may end up seeing a mixed approach–centralized facilities for allogenic therapies, and decentralized for autologous therapies. Both will benefit from robust, highly reproducible methodologies. Given the complexity and cost of cellular therapies, and the regulatory oversight involved with any “first in class” medicines, it makes sense to eliminate sources of error or variability wherever we find them, and to implement automated, highly validated protocols and tools as soon as possible to help give these therapies the best chance of success.
Rolf Ehrhardt, M.D., Ph.D.
After 10 years growing BioCision into the leading provider of temperature-sensitive sample and drug handling solutions, Dr. Rolf Ehrhardt established MedCision in 2016 in order to focus efforts specifically on the automation of pre-clinical and clinical processes. He has more than 25 years of experience in leadership and innovation in medical research and product development. He has authored more than 40 peer reviewed publications and holds multiple patents. Dr. Ehrhardt earned his M.D. and Ph.D. with distinction from the Technical University of Munich, Germany.
Filed Under: Genomics/Proteomics