To combat antibiotic resistance, scientists need to understand the evolution of bacteria and examine this alongside the characteristics of the populations they infect, according to research published in The Lancet Infectious Diseases.
This study identifies a lineage of the highly contagious diarrhoeal pathogen, Shigella flexneri serotype 3a, which is spreading across continents as a sexually transmitted infection of men who have sex with men (MSM). The study, which included Shigella samples from interviewed patients, also shows how this unique transmission pattern has led to the development of unexpected antibiotic resistance characteristics in the pathogen.
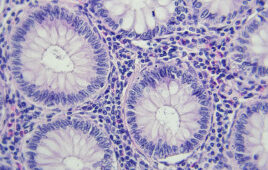
Shigella can be thought of as a traditional diarrhoeal disease affecting regions with poor sanitation or hygiene, most commonly in children under the age of five. However, since the 1970s, it has also been shown that Shigella is a sexually transmissible infection in MSM. Each of these patient groups, traditional and emerging, will expose bacteria to different evolutionary pressures, including different transmission routes and antibiotic therapies.
This study demonstrates the importance of understanding these community characteristics in order to combat the global public health threat posed by highly infectious bacterial diseases that are resistant to antibiotics.
“When it comes to understanding antibiotic resistance, we need to consider who the bug is infecting, and what their history is,” said Dr Kate Baker, first author from the Wellcome Trust Sanger Institute. “Every type of bacterium in our bodies is exposed to the antibiotics we take, not just the particular one we want to battle. Holistic studies like this, where we speak to people and explore their medical histories enable us to understand how bacterial strains transmit globally and why they pick up resistance elements.
Our study highlights the level of detail required to fully understand antimicrobial resistance in order to tackle it and the collateral damage we cause when we take antibiotics.”
Patient samples of Shigella flexneri 3a collected from the United Kingdom and France between 2004 and 2013 (including samples from the UK’s MSM community), and samples from MSM-related outbreaks in other low-risk regions such as Australia and Canada, were compared with samples from patients who contracted Shigella in traditionally high-risk regions such as Asia and Africa. Researchers found a clear genetic lineage of the bug that came from patients who hadn’t travelled to high-risk areas and were mostly middle-aged men, many of whom identified as MSM during interviews.
“Locality wasn’t as big a factor as you might expect in connecting these bacteria,” said Professor Nick Thomson, corresponding author from the Sanger Institute. “We observed a specific subtype of bacteria that has become widely distributed in MSM communities across the globe in less than 20 years. It goes to show that the people we interact with, our community, and not necessarily the people we live next door to, that have the greatest influence on the pathogens we encounter.”
Within the genetic code of these Shigella bacteria, an unusual antibiotic resistance kept appearing. While researchers would expect to come across resistance to ciprofloxacin, the primary antibiotic treatment for diarrhoea caused by Shigella, they found resistance to another antibiotic, azithromycin. Azithromycin is often used in the treatment of sexually transmitted infections such as gonorrhoea, syphilis and chlamydia, which were commonly reported by an interviewed sub-set of MSM in the UK who were infected with the new Shigella lineage. This led researchers to hypothesise that it was the emergence of Shigella as a sexually transmitted illness in a patient group with a high incidence of other sexually transmitted infections that has led to the development of this unusual antibiotic resistance.
In addition to lessons for global antimicrobial resistance, detecting this specific lineage highlights the need for public health organisations to target their interventions at community-based risk groups. Public Health England, in collaboration with the Terrance Higgins Trust, has already implemented a poster campaign to raise awareness that Shigella can be sexually transmitted, how transmission can be prevented and how to spot the symptoms.
“This is an interesting study that appears to confirm from a genetic perspective that Shigella is sexually transmitted in this population,” said Dr Shaun Griffin, Exec Director of External Affairs at the Terrence Higgins Trust. “Shigella is a really serious gut infection causing severe, prolonged diarrhoea and stomach cramps which we’re seeing passed on sexually amongst men who have sex with men (MSM), particularly those living with HIV. MSM with severe symptoms of food poisoning 1-3 days after sex should visit their doctor, mentioning Shigella and ask for a stool test. Shigella is treatable with antibiotics.”
Source: Wellcome Sanger Institute
Filed Under: Genomics/Proteomics